CAR-T for lupus: the ‘tip of the iceberg’ for cell therapy in autoimmune disease
The clue came, as they often do, from an unexpected source. Two years ago, a small study of five people in Germany pointed to a new direction for the high-profile field of cell therapy.
The study showed a cellular medicine could drive a tough-to-treat form of lupus into remission. While early, the finding suggested a technique used to create powerful cellular treatments for cancer might also work against autoimmune conditions like lupus, too.
“It’s very early days, but it’s exciting for the field to see this possibility,” said cell therapy pioneer and University of Pennsylvania immunologist Carl June, in an interview at the time.
The biopharmaceutical industry took note. Since the paper was published, a number of drugmakers have revealed plans to develop cell therapies for lupus, and a dozen or so are now in clinical testing.
Updated results from that German study, presented at a medical meeting in December 2023, indicate they may be right to invest. Among 15 people who had lupus or one of two other autoimmune diseases and hadn’t responded to prior treatment, all were in remission after receiving cell therapy. Some responses have lasted two years.
“It’s the tip of the iceberg, but it looks extraordinary,” said Andy Plump, Takeda Pharmaceutical’s head of research, in a recent interview. “The hope is that this can expand to not just other refractory autoimmune diseases, but to more common diseases.”
Challenges remain. Current cell therapies for cancer are associated with side effects that in rare cases can be fatal, a risk that’s easier to accept for people with deadly tumors than those with chronic health conditions. They’re also complex to produce and administer, and only available at major treatment centers, limiting their potential for wider use. Some believe newer “off-the-shelf” alternatives may be a better fit.
Answers could come within the next few years from clinical trials just getting underway. At least a dozen studies run by startups, biotechnology companies and large pharmaceutical giants are either recruiting participants or soon will be. Here’s where the field stands:
How is lupus treated now?
Lupus is a chronic autoimmune condition that occurs when the body attacks itself. The disease leads to pain and inflammation in many parts of the body, from the skin and joints to internal organs like the kidneys or lungs. About 1.5 million people in the U.S. and 5 million worldwide have a form of the disease, according to the Lupus Foundation of America, a patient advocacy group. For reasons that aren’t quite clear, many of those affected are women of childbearing age. Researchers aren’t certain what triggers the disease in the first place, either.
Lupus has several types, the most common of which is known as systemic lupus erythematosus, or SLE. It affects multiple organs and can involve a constellation of symptoms, making it tough to diagnose. Lupus’ characteristic ‘flares’ arrive unpredictably and can last days or weeks. While most people can manage their disease and live a long life, the condition can result in kidney failure or death from heart-related complications.
There is no cure. Available treatments can help manage symptoms and counteract the immune response associated with the disease. They include repurposed anti-inflammatory or immunosuppressive therapies, steroids or antimalarials.
More recently, three medicines specifically developed for lupus — GSK’s Benlysta, Aurinia Pharmaceuticals’ Lupkynis and AstraZeneca’s Saphnelo — have reached market. Roche’s cancer drug rituximab is sometimes used off-label as well, despite disappointing clinical results.
All have limitations, however. Not everyone responds to treatment and patients can continue to have flare-ups, requiring them to try different treatments. Additionally, drugs that blunt the immune system, like steroids, can leave patients vulnerable to infection.
How could cell therapy be used?
Six so-called CAR-T cell therapies are approved in the U.S. to treat leukemia, lymphoma and multiple myeloma. When they work, these therapies can lead to long-lasting benefit.
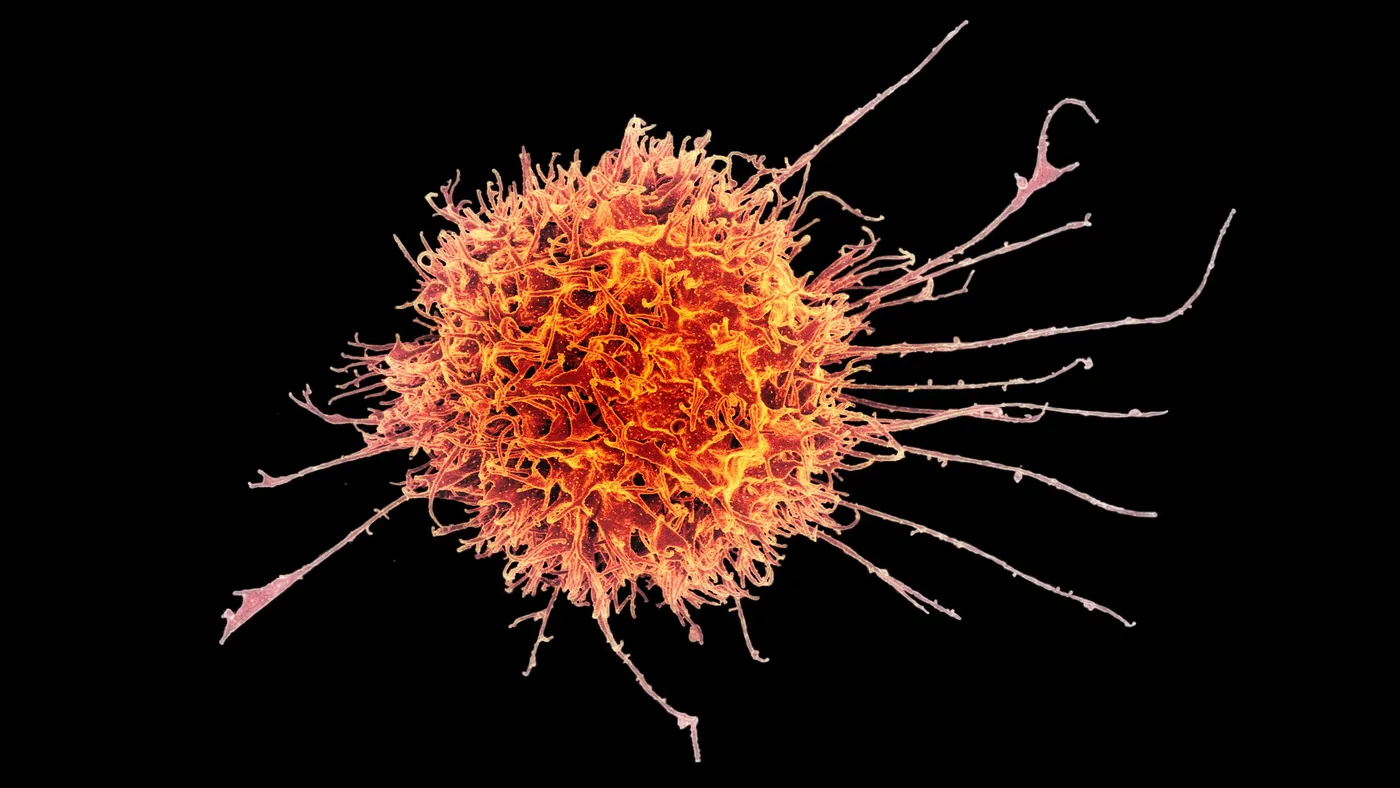
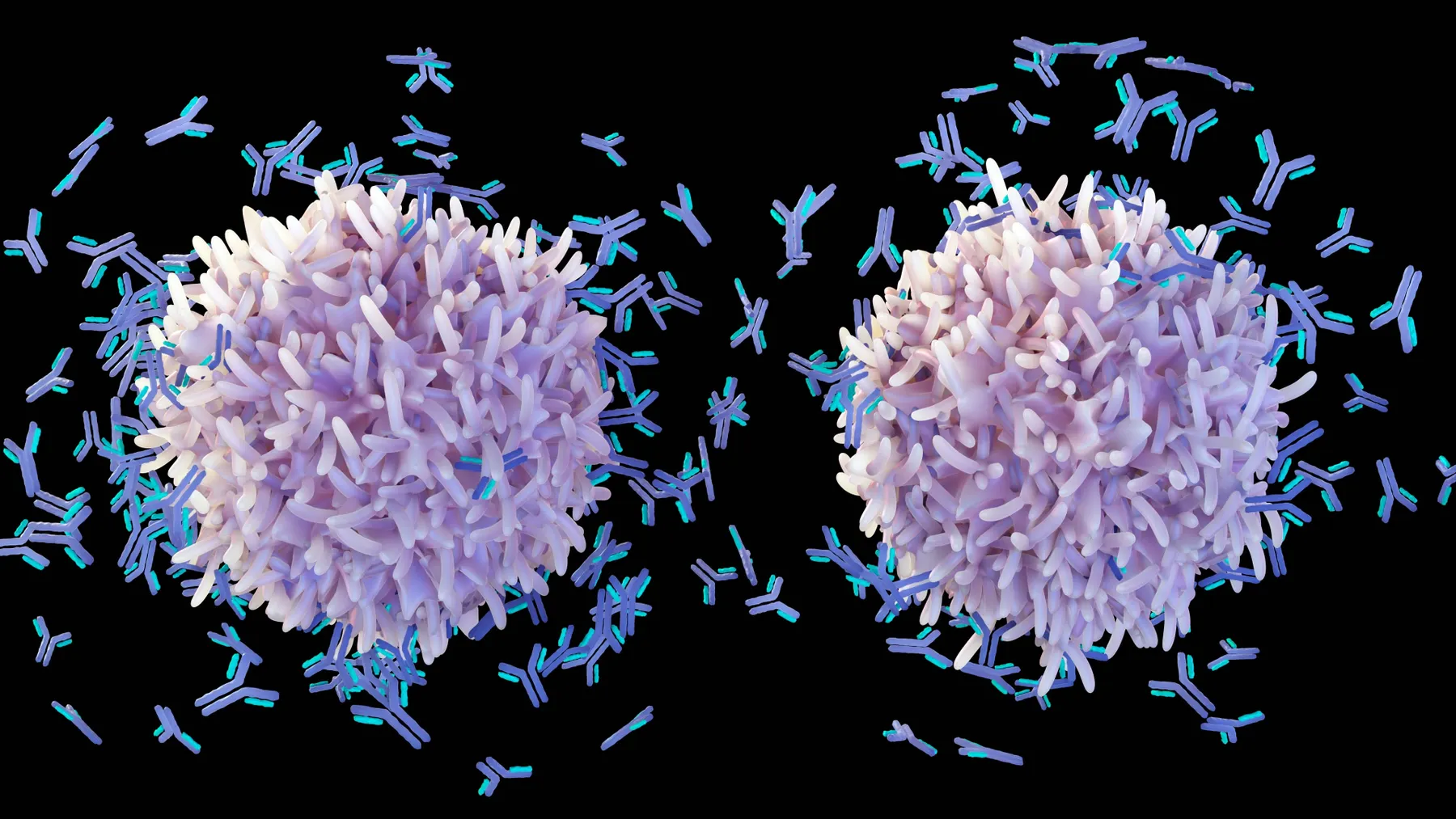
They’re made by genetically modifying a patient’s immune cells to spot proteins found on the surface of cancerous B cells. These cells, which normally make protective antibodies, are also implicated in an array of autoimmune diseases. In lupus, for example, B cells go haywire and make antibodies that damage healthy tissue.
CAR-T therapies wipe out B cells, whether cancerous or not. That effect led Georg Schett and colleagues at the Friedrich Alexander University, Erlangen-Nurnberg, to test CAR-T therapy in people with lupus.
Schett’s team published a case report in The New England Journal of Medicine in 2021, following up one later with results in four more study volunteers, which were presented in Nature. They found the drug depleted B cell counts and drove participants’ disease into remissions that persisted without using other drugs.
Notably, treated individuals still responded to vaccines and their levels of infectious disease antibodies “largely remained intact,” wrote analysts at the investment bank William Blair, in a recent report. Side effects were mild.
When B cells did regenerate, disease symptoms didn’t return, which the authors suggested could support the idea that CAR-T therapy “reboots” the immune system.
To drugmakers, the findings indicate cellular therapies, if engineered right, could potentially cure some autoimmune diseases.
“There's a huge potential for patients to really benefit,” said Samit Hirawat, the chief medical officer of Bristol Myers Squibb, in a recent interview.
Yet it’s still unclear how long responses will last, or whether people may need to be re-treated later. The results may not be replicated as CAR-T therapies are studied in large groups of people with lupus, either.
CAR-T also involves a chemotherapy “conditioning” regimen to prepare patients for therapy. And treatment can cause serious immune and neurological side effects that, in an autoimmune disease setting, “will not be acceptable to patients and physicians,” wrote William Blair analysts.
More seriously, the Food and Drug Administration recently issued safety warnings for all six available CAR-T therapies, following a review of reports of patients developing secondary malignancies after treatment.
Those risks will require developers to mitigate CAR-T’s known safety issues. Companies working on adapting the therapies say their goal is to fine-tune the approach for use in autoimmune diseases.
“I think the whole industry is asking: how can we work on the benefit-risk profile and the conditioning process so that, ideally, you can [treat patients] earlier and earlier and not wait until they have severe, refractory disease?” said Victor Bulto, head of Novartis’ U.S. division.
Which companies are working on cell therapies?
About a dozen companies have launched trials testing cell therapies in lupus, according to a federal database. At least another six have received Food and Drug Administration clearance to begin initial studies and could soon follow, while others still have disclosed plans for testing.
Two cell therapy leaders, Novartis and Bristol Myers Squibb, started Phase 1 trials last year. They’re each testing newer versions of the products they brought to market for cancer, tweaking them to cut manufacturing times, boost safety and raise potency.
Bristol Myers’ Hirawat noted how Schett’s research suggests developers can deliver benefit in lupus with lower and, theoretically, safer doses than in cancer. That’s partly because there are fewer B cells to target in lupus than there are cancerous cells in lymphoma or leukemia.
“We don't anticipate, or want to see, the same safety profile as you saw in malignancies,” he said.
Select lupus cell therapies in federally listed clinical trials
| Company | Cell therapy | Development phase | Trial number | Indication |
|---|---|---|---|---|
| Kyverna Therapeutics | KYV-101 | Phase 1 | NCT05938725 | Lupus nephritis |
| Gracell Biotechnologies | GC012F | Phase 1 | NCT05858684 | SLE |
| Novartis | YTB323 | Phase 1/2 | NCT05798117 | SLE |
| Bristol Myers Squibb | CC-97540 | Phase 1 | NCT05869955 | SLE |
| Cartesian Therapeutics | Descartes-08 | Phase 2 | NCT06038474 | SLE |
| Miltenyi Biomedicine | MB-CART19.1 | Phase 1/2 | NCT06189157 | SLE |
| ImmPACT Bio | IMP-514 | Phase 1/2 | NCT06153095 | SLE and lupus nephritis |
| iCell Gene Therapeutics | BCMA-CD19 cCAR-T | Phase 1 | NCT05474885 | SLE |
| Cabaletta Bio | CABA-201 | Phase 1/2 | NCT06121297 | SLE and lupus nephritis |
| JW Therapeutics | Relma-cel | Phase 1 | NCT05765006 | SLE |
SOURCE: clinicaltrials.gov, companies
Alongside Bristol Myers and Novartis is Kyverna Therapeutics, a well-funded biotech startup that went public in February. Kyverna’s lead program was licensed from the National Institutes of Health and, like that of its larger rivals, targets the protein CD19.
Also in testing are Gracell Biotechnologies, which AstraZeneca acquired last year, Cartesian Therapeutics and startups Cabaletta Bio and ImmPACT Bio. Behind them are an array of cell therapy companies that have said they will go after lupus and other autoimmune diseases, like Fate Therapeutics, CRISPR Therapeutics and Autolus Therapeutics.
China-based biotechs and academic researchers are investing in lupus research, too. A federal database shows nearly a dozen academic or industry-backed trials underway, including studies run by JW Therapeutics, Shanghai GeneChem and Chongqing Precision Biotech.
Some that haven’t publicly announced trial plans, like Takeda, are interested: “Even though we're very far behind, we still think that we have a path,” Plump said.
One reason: Not everyone is pursuing the same approach. Some companies have cell therapies that target BCMA, another protein on B cells, as well as CD19. Some are looking at different targets. And others are changing out components to boost potency, or are tweaking conditioning regimens.
Meanwhile, companies like Artiva Biotherapeutics, Fate, and Sana Biotechnology are trying approaches that rely on the cells of healthy donors. These so-called allogeneic treatments have struggled as cancer therapies. But some developers claim they may have an edge over personalized, or “autologous,” treatments in autoimmune conditions. Here, they say, the advantages of donor-derived therapies like cheaper production costs or lower rates of side effects will be more important.
“Autologous cell therapy for autoimmune [disease] is going to be pretty challenging,” said Carlo Rizzuto, managing director at Versant Ventures, a venture firm that invested in allogeneic cell therapy developer Century Therapeutics. “I do think that allogeneic off-the-shelf approaches, especially the stem cell-based approaches, will have an advantage.”
Cell therapies could also face competition from newer antibody drugs designed to better deplete B cell counts. Roche and Johnson & Johnson, for instance, have drugs in mid- or late-stage testing for lupus.
“We will have to see how science evolves across all these modalities and see which one works best for which patients,” said Bulto, of Novartis.
Select cell therapies for lupus cleared for testing by FDA*
| Company | Cell therapy | Development phase | Trial number | Indication |
|---|---|---|---|---|
| Nkarta | NKX019 | To be confirmed | Not yet listed | Lupus nephritis |
| Sana Biotechnology | SC291 | Phase 1 | Not yet listed | Lupus nephritis |
| Artiva Biotherapeutics | AB-101 | To be confirmed | Not yet listed | SLE and lupus nephritis |
| Century Therapeutics | CNTY-101 | Phase 1 | Not yet listed | SLE |
| Luminary Therapeutics | LMY-920 | Phase 1 | Not yet listed | SLE |
| Fate Therapeutics | FT-819 | Phase 1 | Not yet listed | SLE |
*Describes instances when the FDA has cleared an Investigational New Drug application, but no trial is listed in clinicaltrials.gov database. SOURCE: companies
What’s next?
Several clinical trial readouts this year and next could build on Schett’s study. The tests underway are enrolling patients with SLE or lupus nephritis, when the condition affects the kidneys. Some developers are recruiting people with other autoimmune conditions as well, which could provide more clues as to how broadly cell therapy might be applied.
Kyverna presented early results from a lupus nephritis study last year and is recruiting patients. A fuller readout could come in 2025, according to a federal database. The company is planning to test its treatment in systemic sclerosis, myasthenia gravis and multiple sclerosis, too.
Novartis shared preliminary findings last year in a study testing its therapy, YTB323, in SLE. More data are expected in the second half of 2024. Bristol Myers should provide an early look at its program’s potential this year, too, and intends to expand into MS, myositis and other conditions.
Others, such as Fate, Nkarta and CRISPR intend to start dosing patients in 2024. Startups with different approaches, like Luminary Therapeutics, could follow afterwards.
Some of these efforts will need to bear fruit for investment to continue at such a torrid pace. CAR-T’s potential in lupus alone “can't sustain this massive energy” in the industry, Plump said. “There are pieces that we're just starting to work through, but it's an area of a lot of excitement.”