Dive Brief:
- The Federal Trade Commission has released a second report examining how pharmacy benefit managers may be inflating drug costs in the U.S., in the latest and likely last salvo by antitrust regulators in the Biden administration against the drug supply middlemen.
- The report accuses CVS’ Caremark, Cigna’s Express Scripts and UnitedHealth’s Optum Rx of hiking the price of life-saving drugs by hundreds or thousands of percent. The so-called “big three” PBMs also directed the most profitable prescriptions to affiliated pharmacies at the expense of independent operators, and paid themselves more than other pharmacies for dispensing drugs, the report says.
- The findings are similar to those in the FTC’s initial report released last summer. However, the second report looks at a broader array of drugs after the first report was criticized for relying on too little data. FTC commissioners voted unanimously to release the report Tuesday.
Dive Insight:
Three years ago, the FTC launched an inquiry into PBMs, which negotiate with pharmaceutical companies for discounts on drugs and pay pharmacies for dispensing them.
PBMs claim they save plans and patients money by pressuring drugmakers to lower the cost of drugs. However, the FTC’s first report found consolidation has resulted in a few major players wielding outsized influence to profit at the expense of patients and independent pharmacies.
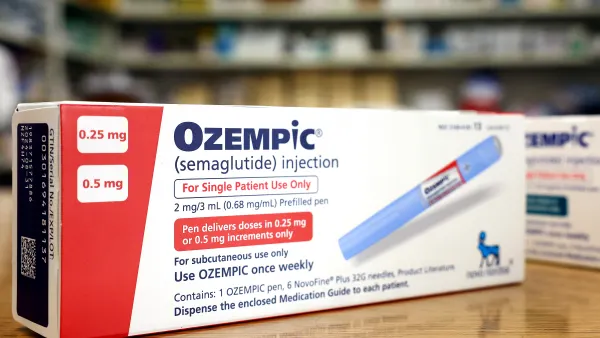
Two months later, the agency leaned on the report to sue Caremark, Express Scripts and Optum Rx, which jointly account for 80% of U.S. prescriptions, and alleged they artificially inflated the cost of insulin.
However, the PBM industry, along with the agency’s two Republican commissioners and some pharmacy market experts, took issue with the report, arguing it was one-sided and relied on cherry-picked data. Members of the big three countersued the FTC and called on FTC Chair Lina Khan and two Democrat-appointed commissioners to recuse themselves from the agency’s lawsuit.
Specifically, the FTC’s first report found Caremark, Express Scripts and Optum Rx prioritized access to high-cost drugs in return for larger discounts from drugmakers and gave their own pharmacies preferential treatment. But the report’s findings relied on just two specialty generic drugs used to treat cancer.
The second report released Tuesday analyzes a significantly larger set of drugs after PBMs shared more data, according to the agency.
The FTC looked at all specialty generic drugs dispensed from 2017 to 2022 for people in commercial health plans and Medicare prescription drug plans managed by Caremark, Optum Rx and Express Scripts. The resulting data set includes more than 50 medicines.
According to the report, the three companies marked up specialty generic drugs dispensed at affiliated pharmacies beyond their estimated acquisition costs, generating $7.3 billion in additional revenue from 2017 to 2022.
The problem is “growing at an alarming rate,” Hannah Garden-Monheit, the director of the FTC’s Office of Policy Planning, said in a statement. FTC staff noted the estimated $7.3 billion markup is likely an underestimate due to how acquisition costs are measured.
Caremark, Express Scripts and Optum Rx reimbursed affiliated pharmacies at a higher rate than unaffiliated pharmacies on nearly every specialty generic drug investigators analyzed.
Spokespeople for Caremark and Express Scripts said they were still reviewing the report, but that it’s misleading to focus on specialty generic products, which represent a small portion of clients’ overall drug spend.
The FTC also ignored cost-saving guarantees PBMs provide clients, according to Caremark.
“How many more interim reports will it take before the FTC includes the mountain of data that refutes these few outliers? We’ve provided terabytes of data in compliance with their requests, and virtually none of that data is reflected in this report,” David Whitrap, CVS’ vice president of external affairs, said in an emailed statement.
A spokesperson for Optum Rx said the company is focused on lowering the cost of specialty drugs and supporting patients with complex and rare conditions.
The FTC’s decision to release the report comes six days before the swearing in of President-elect Donald Trump ushers in an administration expected to dial back the Biden administration’s antitrust agenda.
Trump plans to name current Commissioner Andrew Ferguson as FTC chair and appoint Mark Meador, an antitrust lawyer and former congressional staffer, to fill Khan’s expected vacancy. (Khan’s term expired in September, but she can stay on until she's replaced, which is expected soon after Trump assumes office.)
The change could benefit PBMs: Commissioner Ferguson recused himself from the FTC’s lawsuit against the drug middlemen, arguing it represented an overreach of the agency’s power.
Yet both Ferguson and Melissa Holyoak, the other Republican commissioner, voted to release the second report on Tuesday, suggesting bipartisan support for future efforts. And recent statements by Trump have created more uncertainty for the drug middlemen. In December, the president-elect said he planned to “knock out the middlemen,” referencing PBMs.
There’s also momentum in Congress to curb drug costs by addressing PBM business practices. A bipartisan group of lawmakers proposed legislation to break up PBMs in December, while PBM reform almost made it into year-end spending package that was later scuttled by Trump.