For all the clinical success of cancer drugs like Merck & Co.'s Keytruda, a good number of patients still don't see a major benefit from immunotherapy. Finding a way to expand the share who do has become the chief objective of drugmakers in the space, many of which have centered efforts on studying new treatment combinations.
Some eleven hundred clinical studies are currently testing cancer immunotherapies together with a kaleidoscope of chemotherapies, targeted drugs and other agents designed to recruit the immune system to attack tumors.
This spring, however, investor attention will center on just one: a Phase 3 study pairing Merck & Co's PD-1 inhibitor Keytruda with an experimental therapy developed by Incyte Corp. in patients with metastatic melanoma.
Initial results could come by May and hold the potential to hand Merck another edge in immuno-oncology. If the trial succeeds, Incyte's drug could become a partner of choice for PD-1/L1 blockers in certain cancers. A failure, on the other hand, would likely shave down the biotech's roughly $20 billion market capitalization.
For a still-unsettled immunotherapy field, the study results will also deliver some answers — and potentially more questions — about how best to combine immunotherapies with other drugs.
Blocking IDO
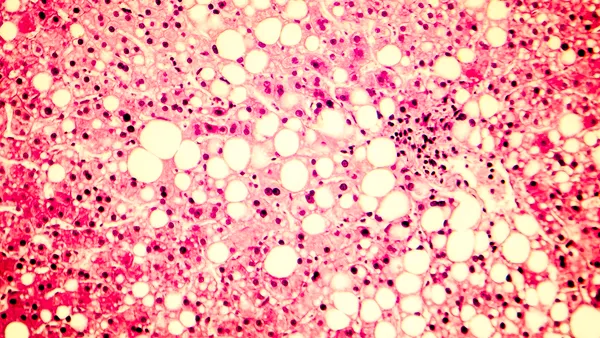
Epacadostat, as Incyte's drug is known, blocks an enzyme called IDO1 and is seen as complementary to the checkpoint inhibitors that have pushed immuno-oncology forward.
Upregulation of IDO1 alters the so-called tumor microenvironment, suppressing some T-cell function and enabling tumor cells to disguise themselves from an immune response. Inhibiting IDO1 seems to reverse that immunosuppressive effect and enhance the ability of T-cells to target cancerous cells.
PD-1/L1 blockade also works by boosting immune response to cancer, but does so through inhibiting the action of a checkpoint molecule by the same name.
"It is a reasonable scientific construct to make an assumption that an IDO inhibitor could improve an outcome where a PD-1 inhibitor already has activity, rather than looking to see if an IDO inhibitor can convert a non-responsive tumor," said Roger Dansey, therapeutic area head of oncology late-stage development at Merck Research Laboratories, in an interview.
That logic leads directly to melanoma, an area where PD-1/L1-targeted immunotherapies have already advanced standards of care.
Proving ground for immunotherapies
Each of the first three checkpoint inhibitors approved in the U.S. — Bristol-Myers Squibb Co.'s Yervoy (ipilimumab) and Opdivo (nivolumab) as well as Merck's Keytruda — entered the market to treat advanced melanoma.
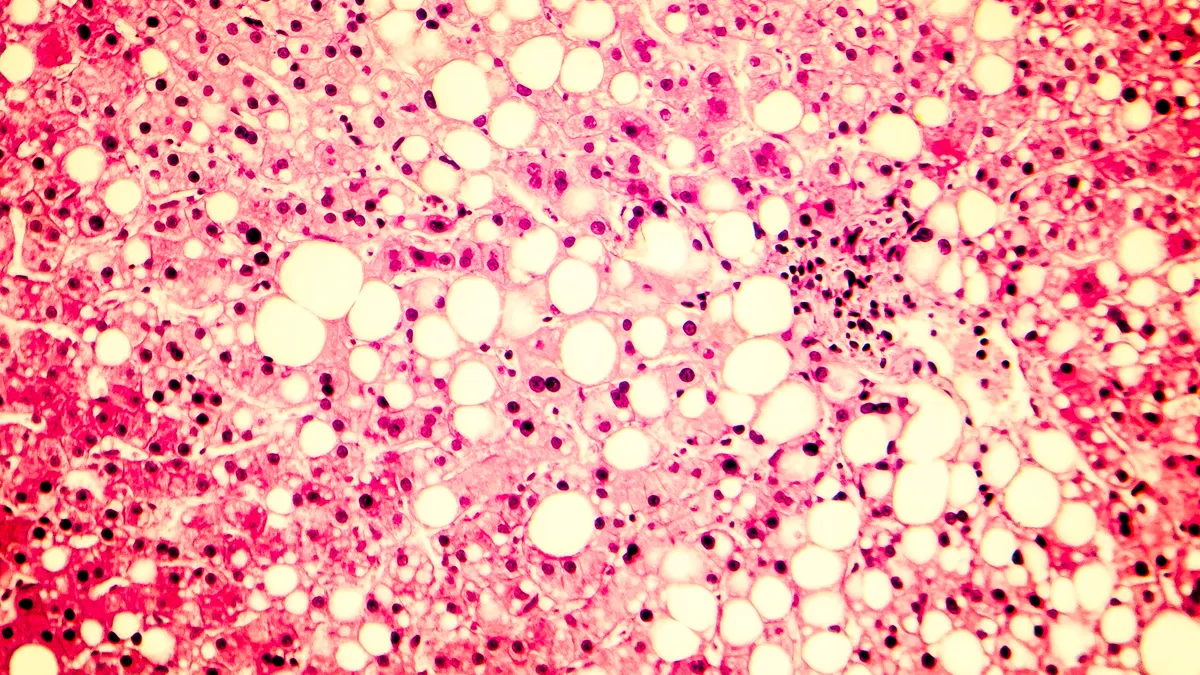
Melanoma is particularly suited for treatment with immunotherapy due to the immuno-reactive nature of the skin cancer. Yervoy, which blocks a checkpoint molecule called CTLA-4, won U.S. approval in 2011, followed by Keytruda and its rival PD-1 inhibitor Opdivo in 2014.
"Melanoma is certainly the guidepost for these immunotherapies," explained Aiman Shalabi, chief medical officer at the Cancer Research Institute (CRI), a non-profit that funds cancer research.
Keytruda or Opdivo monotherapy is currently considered the standard of care in first-line treatment of metastatic melanoma. A combination of Opdivo plus Yervoy set an even higher bar in extending median progression-free survival (PFS), notching an 8.6 month improvement over Yervoy alone and a 4.6 month boost over Opdivo monotherapy.
Adding Yervoy, however, results in higher toxicity, with nearly three-quarters of patients tested in a Bristol-Myers' study experiencing a Grade 3 or 4 adverse event.
"Melanoma is certainly the guidepost for these immunotherapies."

Aiman Shalabi
CMO, Cancer Research Institute
Merck's interest in epacadostat grew after early uncontrolled data suggested adding the drug could improve upon Keytruda's clinical profile. Results from the small study, which were updated in September, showed the combo appeared to lead to higher response rates and median progression-free survival with a still manageable safety profile.
"Melanoma is a good starting point because of the clear efficacy and value that pembrolizumab brings to melanoma," said Merck's Dansey. "If you can improve on that outcome and not add a safety burden, that would be a good thing for patients. I think that's what this initial trial should be able to answer for us."
Looming readout
In addition to testing the two drugs in melanoma, Merck and Incyte announced last spring plans for Phase 3 studies of the combo across kidney, head and neck, lung and bladder cancers.
PD-1/L1 combination studies involving epacadostat
| Combination | Cancer type | Partner | Trial name |
|---|---|---|---|
| Epacadostat + Keytruda | Melanoma | Merck | ECHO-301 |
| Epacadostat + Keytruda | Renal cancer | Merck | ECHO-302 |
| Epacadostat + Keytruda | Bladder cancer | Merck | ECHO-303 & -307 |
| Epacadostat + Keytruda | Head & neck cancer | Merck | ECHO-304 |
| Epacadostat + Keytruda | NSCLC | Merck | ECHO-305 & -306 |
| Epacadostat + Opdivo | NSCLC | Bristol-Myers Squibb | ECHO-309 |
| Epacaodstat + Opdivo | Head & neck cancer | Bristol-Myers Squibb | ECHO-310 |
| Epacadostat + Imfinzi | NSCLC | AstraZeneca | Expected to start H1 2018 |
ECHO-301, as the study pairing epacadostat and Keytruda in melanoma is known, will be the first of Merck and Incyte's late-stage studies to read out data.
Topline numbers on Keytruda and epacadostat's effect on progression-free survival are expected to be disclosed. The study will also test the combination's ability to extend overall survival, although that data won't be fully available by this spring.
If ECHO-301 hits its goal, Incyte plans to file a New Drug Application sometime in the second half of the year for approval by the Food and Drug Administration.
Building on monotherapy
Beyond determining the success or failure of Keytruda plus epacadostat in melanoma, ECHO-301 is also relevant for the broader surge in investment into testing combination therapies.
Checkpoint inhibitors can deliver dramatic results in some patients, particularly those with high expression of PD-L1 or a greater burden of mutations in their tumors. For others, however, treatment doesn't add significant benefit over current treatments across the range of cancer types for which the drugs are approved.
"Combination therapy is absolutely going to be the rule."

Reid Huber
CSO, Incyte
"PD-1 monotherapy or even PD-1/CTLA-4 antagonism is not driving sufficient benefit. There is a need in the field to build on those regimens," explained Reid Huber, chief scientific officer at Incyte, on a recent call with investors.
"Combination therapy is absolutely going to be the rule, it's not going to be the exception," Huber said.
Twenty-two studies are currently investigating combination treatments involving an IDO inhibitor and 18 of those feature epacadostat in some form, according to data provided by CRI.
Both Bristol-Myers Squibb and AstraZeneca plc have also lined up trials pairing their respective PD-1/L1 inhibitors with epacadostat.
And while Incyte's epacadostat is the most advanced IDO inhibitor, another biotech called Newlink Genetics Corp. is advancing a candidate that also blocks the IDO pathway. Early Phase 2 results released in 2017 showed Newlink's drug paired well with Keytruda in advanced melanoma.
"The question is, if [ECHO-301] fails will that cool any of the enthusiasm? Some believe it will and others believe it will just remove one competitor and create a more attractive, uncompetitive environment for the other ones in the field," noted Evercore ISI analyst Josh Schimmer in an interview.
"It can cut both ways. I doubt failure would really chill cancer I/O in general, but it would certainly chill IDO inhibitors."
To Schimmer's point, CRI data shows that IDO is only the seventh most common partner for PD-1/L1 inhibitors among the 1,100 or some combination studies counted by the non-profit. Pairing with chemotherapy, CTLA-4 blockade and radiotherapy are all more popular avenues of study, for example.
A negative readout from ECHO-301 could also make Bristol-Myers recent decision to commit $1.85 billion upfront for partial rights to an experimental drug from Nektar Therapeutic Inc. look a whole lot smarter. Nektar's drug, called NKTR-214, also alter the tumor microenvironment but does so by expanding the number of T cells and natural killer cells present.
Market impact
For the first few years on the market, Bristol-Myers' Opdivo set the pace in cancer immunotherapy, running up a large lead in overall sales.
Keytruda has since drawn even, due in part to approval of Keytruda together with the chemotherapy pemetrexed as a first-line lung cancer treatment in the U.S. More than half of Keytruda revenues now come from prescriptions for lung cancer, compared to only about a fifth attributable to use in melanoma.
With ECHO-301, Merck could gain another step on the cancer immunotherapy field yet again. A study miss would set back one of its major combination bets, but likely wouldn't derail the pharma's overall strategy given recent collaboration deals with AstraZeneca and Eisai Co. Ltd.
For Incyte, on the other hand, the results of ECHO-301 will have a much more noticeable impact.
"Much of [Incyte]'s valuation is tied to the epacadostat opportunity across various oncology indications," wrote Leerink analyst Michael Schmidt in a recent report, noting the ECHO-301 results would likely have a binary effect on the company's share price.
Incyte stock has slowly slid downwards in value since a peak in early 2017, yet still commands an overall capitalization that nearly ranks among the top ten for biotechs publicly listed in the U.S.
Since 2014, the cancer immunotherapy field has seen several swings in corporate fortune. Come May, Incyte and Merck could be at the center of another.