In the early 1980s, a pair of Australian researchers discovered an unlikely carcinogen.
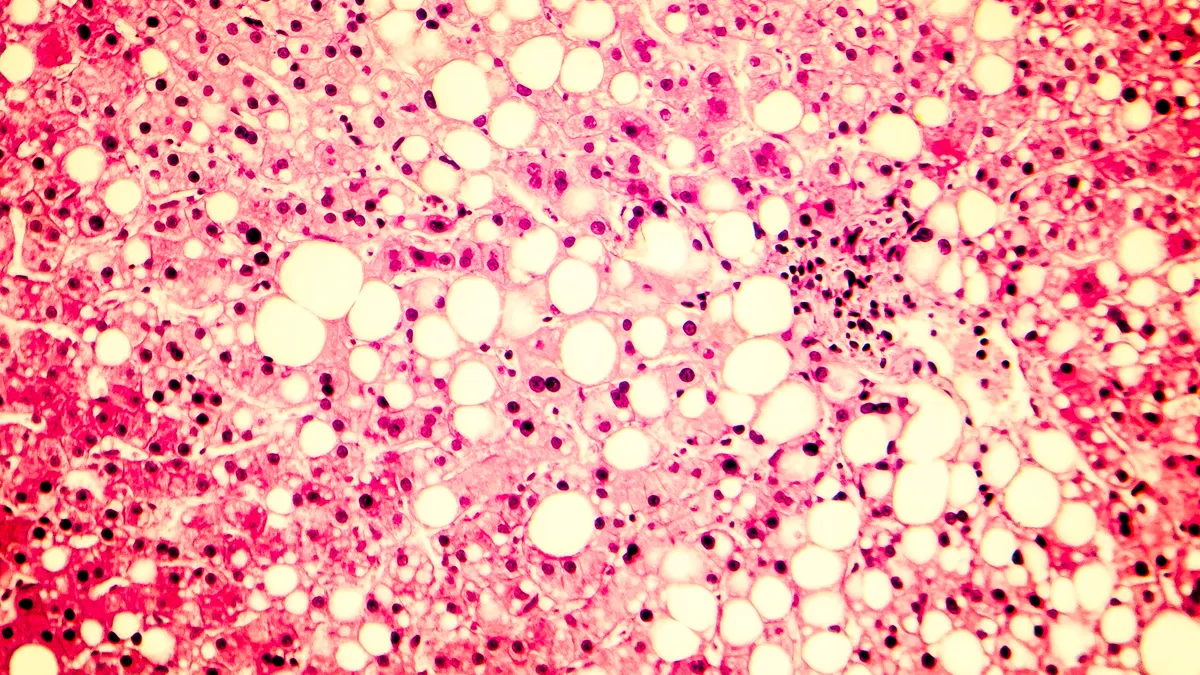
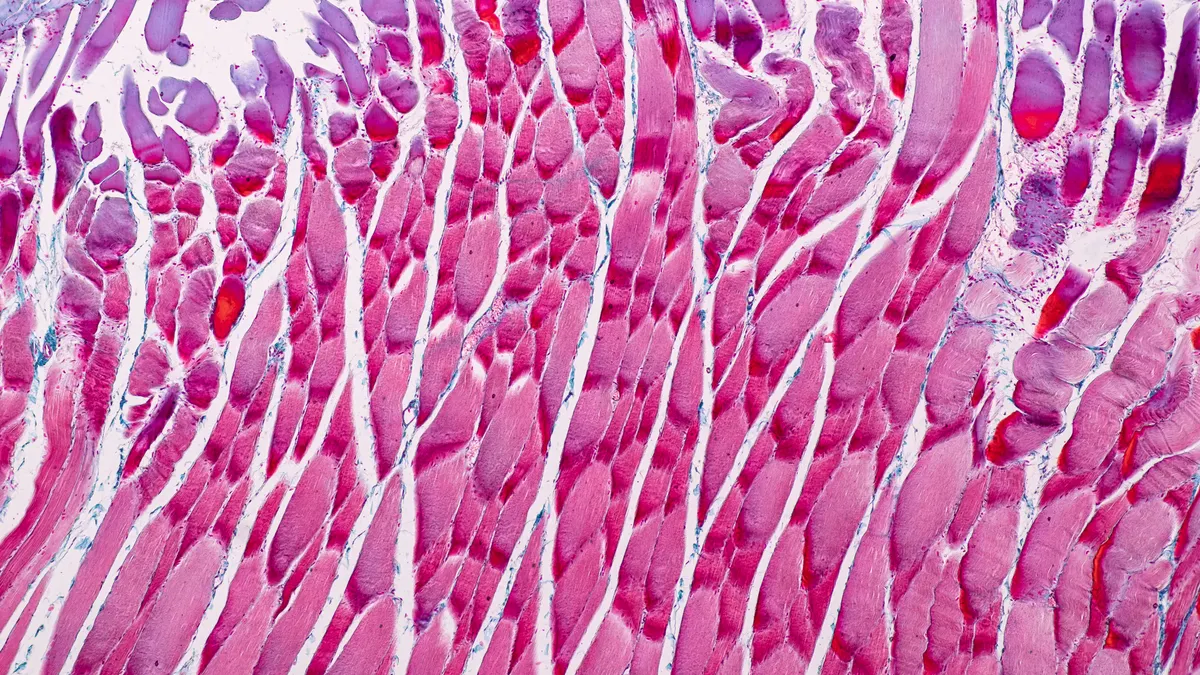
Barry Marshall and Robin Warren identified a previously unknown bacteria that — contrary to the thinking of the time — could take root in the gut. Dubbed Helicobacter pylori, this microorganism proved the missing trigger behind stomach inflammation known to heighten the risk of stomach cancer.
Their work occurred during a decades-long hunt for mechanistic causes of cancer. Now, emerging understanding of the trillions of bacteria living in the gut has led to new exploration of the relationship between bacteria and cancer.
"The role of microbes as it relates to cancer is not new," said David Berry, general partner at Flagship Pioneering, in an interview. "Despite the fact that it feels new because it has been renewed and we are looking at it in an entirely new way, it is something we have known foundationally for a long time."
Infectious diseases and inflammatory conditions are the more obvious areas of research into the so-called microbiome. But, as investment grows, the interaction between cancer, bacteria, and the immune system is getting a closer look.
Cancer research involving the microbiome seeks to solve one of immuno-oncology's most vexing questions: Why do some patients respond to cancer immunotherapy while others don't?
Research hints
Research published in the journal Science last November hinted at how inquiry into the relationship between the microbiome and immuno-oncology could bear fruit.
A team at the University of Texas MD Anderson Cancer Center — led by associate professor of Surgical Oncology and Genomic Medicine Jennifer Wargo — found a link between greater diversity of bacteria in the gut and patient responses to anti-PD-1 cancer immunotherapy, a field now led by Merck & Co.'s Keytruda (pembrolizumab) and Bristol-Myers Squibb Co.'s Opdivo (nivolumab).
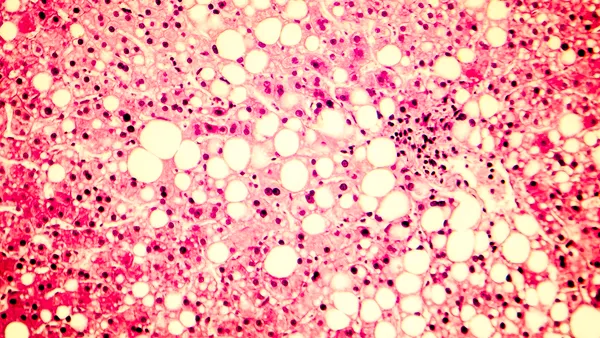
The researchers collected stool samples from patients with metastatic melanoma before and following treatment, comparing the variety and composition of bacteria in those who responded to that of non-responders.
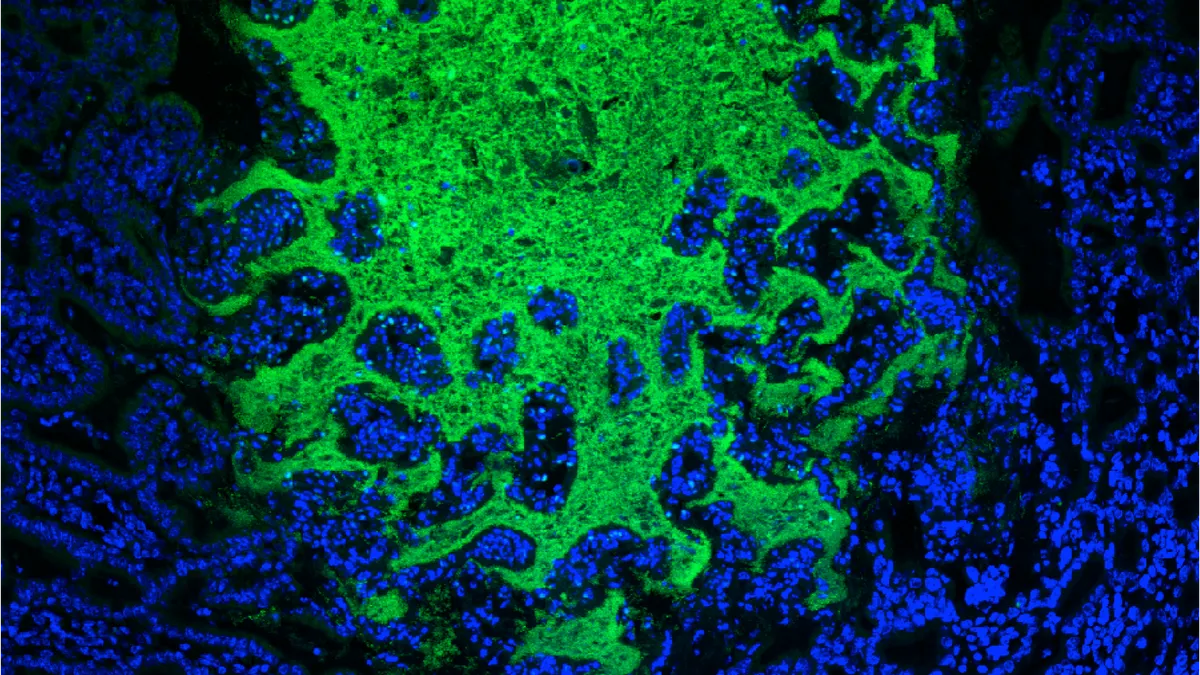
Not only did the team's work show a correlation between a greater mix of microbes and response to immunotherapy, they also identified specific types of bacteria associated with those patients who saw a benefit to treatment. Relative abundance of faecalibacterium and clostridiales bacteria were significantly correlated with greater concentration of cancer-killing T-cells in the tumor microenvironment.
To test whether that correlation could translate into a causal link, the MD Anderson team transplanted stool from immunotherapy responders and non-responders into germ-free mice, who were then injected with melanoma cells. Those mice receiving fecal microbiota transplants (FMT) from responders experienced significantly reduced tumor growth compared to mice given such transplants from non-responders.
"How do you get from the composition of what is in your gut to your immune cells in your tumor?"

Theresa LaVallee
Head of translational medicine, Parker Institute for Cancer Immunotherapy
While the study is small and descriptive, it suggested that altering the composition of the microbiome could help boost the efficacy of immunotherapy. Similar conclusions were reached in a 2015 study in mice by Thomas Gajewski at the University of Chicago.
"[Research] has shown a strong correlation between the microbiome profile and the T-cells and immune state of the tumor," explained Theresa LaVallee, head of translational medicine at the Parker Institute for Cancer Immunotherapy.
The question now becomes how exactly the health of the microbiome influences T-cell activity.
"That is what I would characterize as the black box. How do you get from the composition of what is in your gut to your immune cells in your tumor?" LaVallee said.
Since it appears that microbiome influences the immune system, one hypothesis is that greater diversity could lead to increased antigen presentation — which in turn enhances anti-tumor immune response. If that's the case, patients with more varied gut bacteria or greater abundance of certain types could be better suited to receiving immuno-oncology drugs like checkpoint inhibitors.
Searching for therapeutics
As intriguing as the research is, the current findings are only a starting point. Describing the differences in gut bacteria diversity can only say so much about why patients might respond better to immunotherapy.
"Diversity is an easy thing to measure which is part of why people report on it," explains Flagship's Berry. "It is an initial description. But it doesn't give you a point of actionability. Merely increasing diversity or decreasing diversity is probably not what is driving the response."
Stool samples have their own limitations, too, as they may only reflect part of the microbiome's composition. "If it turns out that melanoma is really being associated with some changes occurring in, say, the proximal [gastrointestinal tract], we might never find it just by looking at the changes that are occurring in the rectum," said Berry.
Even so, publication of Wargo's research was quickly followed by announcement of a partnership between microbiome biotech Seres Therapeutics Inc., MD Anderson and the Parker Institute. Together, the group aims to test an adjunctive microbiome therapy developed by Seres together with a PD-1 inhibitor in a randomized, placebo-controlled study.
"We expect to be in humans this year to ask the question: Can we increase the efficacy of checkpoint inhibitors in people with metastatic melanoma?" Seres CEO Roger Pomerantz said in an interview. (Flagship launched Seres in 2013 and led several venture funding rounds.)
In LaVallee's eyes, the upcoming study will be an important step for informing further clinical research.
"If folks have a bad microbiome and we administer a live bacterial product or FMT, can we then alter the microbiome, change the immune infiltrate in the tumor, and then can we see a therapeutic benefit?" said LaVallee.
"For a first-in-man study, answering questions one and two to show that approach is doable is the most critical."
Under the collaboration, Seres has an exclusive option to license from MD Anderson intellectual property as it relates to the use of bacteria in combination with checkpoint inhibitors.
Pomerantz says that IP position, along with the profile of MD Anderson and the Parker Institute, has attracted interest from big pharma players.
"I would point out that, because of all of this — because we have these groups, because we are able to put drugs into patients, because we do have all of the IP locked up — we are getting great interest from large pharma companies," Pomerantz said.
Pomerantz didn't tip his hand to whether that interest centered on licensing deals or broader collaborations. Yet such interest would fit with the intense interest from immuno-oncology players in finding a way to raise patient response rates.
Seres isn't alone in planning cancer-related studies of the microbiome. Other companies, such as Evelo Biosciences Inc., plan to kick off trials testing microbiome candidates in cancer this year. And big pharma has shown interest, too. Bristol, for example, has inked a cancer-focused research deal with Enterome SA to explore microbiome-derived biomarkers.
Still searching for answers
In the 1980s, Marshall and Warren faced incredulity at the suggestion microorganisms could survive the churning acids in the stomach. Their work not only supported the presence of bacteria in the gut, but pointed to a new carcinogen.
"I think people have realized that this is serious science and making serious drugs."

David Berry
General partner, Flagship Pioneering
Work into the broader microbiome faced similar dismissiveness at first. "When we started … the number of poop jokes I got in investor meetings was quite high," said Berry. " Now, you don't get those jokes anymore and I think people have realized that this is serious science and making serious drugs."
That said, research into the role played by the microbiome in immuno-oncology is still emerging and will take time to confirm and build upon. Many questions — such as whether gut bacteria diversity can raise response rates to immunotherapy — have only incomplete or unclear answers.
Wargo and Gajewski's work will need to be followed up with prospective clinical trials to fish out whether altering the microbiome can indeed boost responses as initial research suggests. And the field still needs better tools to assess the relative health of the microbiome and better distinguish between a 'good' and 'bad' microbiome.
"When you really get down to say, 'Could you have a diagnostic today that has the right robustness and precision as well as cut point as to classify?' That still needs to emerge," said LaVallee.